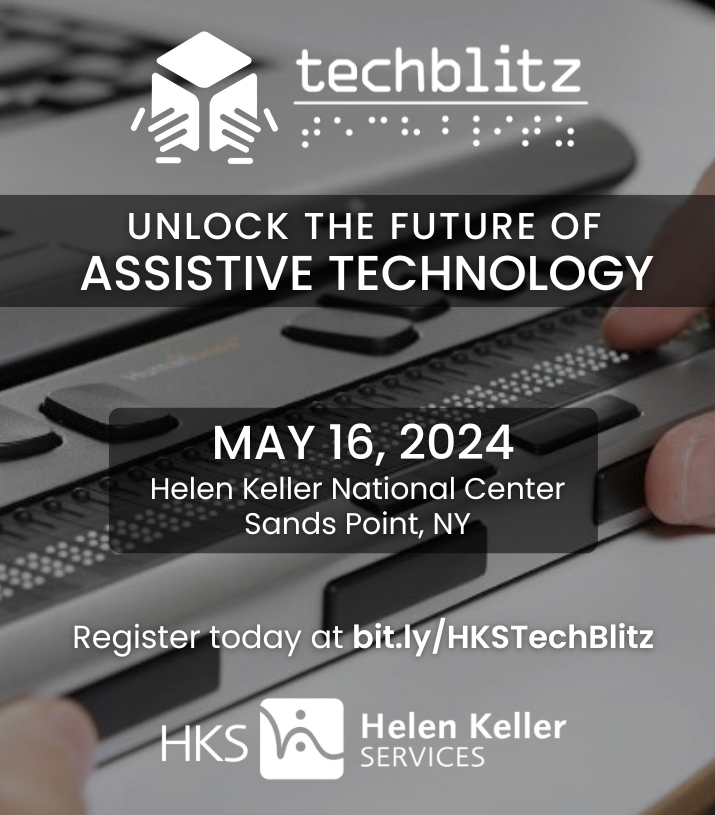
Discover the future of assistive technology at Helen Keller National Center.
HKS Overview
Welcome to Helen Keller Services
Since 1893, we’ve been providing services to individuals who are blind, DeafBlind, have low vision or combined hearing and vision loss to make their own dreams come true.
Our two divisions, Helen Keller Services for the Blind and the Helen Keller National Center for DeafBlind Youths and Adults, provide customized training and support for individuals in the Greater New York area and across the United States.
Our instructors provide personalized training and guidance to each individual. Our clients are true partners in the process, collaborating with staff to design training plans that are tailored to their needs and goals. Everything they learn through HKS has practical, real world applications.
One-on-one coaching, cutting-edge technology, hands-on learning and the chance to interact with people who know firsthand the challenges of living with vision or combined vision and hearing loss—it’s all part of the HKS experience.
Helen Keller National Center for DeafBlind Youths & Adults
We are leading the way in services, support and technology for DeafBlind youth and adults across the United States. Whether you access services through our Long Island, NY, campus, virtually or in your community, you will find the knowledge, innovation and understanding you need to set and achieve your own life goals.

Who is HKNC for?
- People Who Are DeafBlind or Have Combined Hearing and Vision Loss
- Living in the United States and U.S. Territories
- Services for Teens & Young Adults
Helen Keller Services for the Blind
For people experiencing vision loss throughout the greater New York area, we are here to provide the services, training, learning and technology you need to live life to the fullest — from a diverse team that understands your challenges firsthand.

Who is HKSB for?
- People Who Are Blind, Low Vision or with Developmental Disabilities
- New York City/Long Island Area
- Transition Age Youth Through Seniors

On-site & Online Courses
HKNC Learning Center
We believe in life long learning. That is why we offer a broad range of in-person and online courses and other educational resources for professionals who work with individuals who are DeafBlind, or have combined hearing and vision loss, and/or have additional disabilities. We also offer courses and resources for families and individuals who are DeafBlind.
Voices From The Community
I was given my life back as well as my self-reliance and autonomy. Thank you – Helen Keller – for caring enough so I don’t need to live my life with bitterness and anger, but rather joy and anticipation for new things that are yet to touch my life.
Barbara Tucker
I have been able to feel a sense of empowerment in being able to continue developing greater skills for maintaining my independence.
Rebecca Alexander
The workers were always professional, listened to me and my ideas, advocated for me, and made me feel like they were a part of my journey.
Margaret Parker
Join Our Mission
Donors
Goals and dreams can become a reality with your generous donation.
Partners
Our partner network is doing more, together. Bring us your ideas, projects and initiatives and discover how we can work as a team.
Volunteers
Your time is our greatest resource. Volunteers find fulfillment and make a difference every day at HKS.
We are proud to partner with some of the most innovative and progressive individuals and organizations in the country.
News & Events
We have been busy! Find out what we have been up to, and check out what is coming next.